Today we saw a case of a patient with renal transplant who developed CMV esophagitis and also has a newly diagnosed high grade B-cell neoplasm in need of chemotherapy.
This raised a number of questions which I have attempted to answer with the associated references.
1) How do we manage this patient?
2) When can we safely provide cancer treatment?
3) Why did this happen?
The American Journal of Transplantation has a set of guidelines which has recently been updated. The guidelines for CMV prevention and treatment are available here. These guidelines are similar, but in the bone marrow transplant population.
This article looks at risk factors in renal transplantation for developing CMV disease.
This article addresses what happens to patients with pre-existing CMV disease (or recently treated) who go on to SCTx.
Finally, this article describes/summarizes post transplant lymphoproliferative disorder (PTLD) which this patient's lymphoma likely is related to.
(I'm not providing you with medical advice. Clinical correlation and professional interpretation required)
Wednesday, January 27, 2010
Tuesday, January 26, 2010
Choramnionitis with Beta-Hemolytic Strep Bacteremia
Today we discussed a case of presumed choramnionitis with beta-hemolytic strep bacteremia. I have previously blogged about GBS here and peripartum GAS infection here.
This article, while basic, is a reasonable review of the role on parenteral antibiotics in peripartum women with fever. I would probably choose slightly different antibiotics if giving more than one/two doses. This article discusses the differential diagnosis of peripartum fever.
This cochrane meta-analysis questions the practice of peripartum prophylaxis in known GBS patients... I'm still convinced it is a good idea.
This article, while basic, is a reasonable review of the role on parenteral antibiotics in peripartum women with fever. I would probably choose slightly different antibiotics if giving more than one/two doses. This article discusses the differential diagnosis of peripartum fever.
This cochrane meta-analysis questions the practice of peripartum prophylaxis in known GBS patients... I'm still convinced it is a good idea.
Monday, January 25, 2010
Varicella Pneumonia
 Today we saw a case of disseminated varicella with associated varicella pneumonia / pneumonitis. This was in the context of a primary infection in an adult patient.
Today we saw a case of disseminated varicella with associated varicella pneumonia / pneumonitis. This was in the context of a primary infection in an adult patient.This is a review of varicella pneumonitis, and a link to an article discussing the contraversial role of corticosteroids in its treatment.
Varicella can also cause a number of end organ specific syndromes including:
- myopericarditis
- retinitis
- meningitis and meningoencephalitis.
- transverse myelitis
- pancreatitis
- hepatitis
- Ramsey Hunt Syndrome (? role for treatment with antivirals)
- Role for caution with steroids in the absence of antivirals for proven RHS?
- Role for caution with steroids in the absence of antivirals for proven RHS?
There are guidelines of management and a good review of various syndromes published here.
Previous related blogs are here and here.
Thursday, January 21, 2010
Clostridium difficile smorgasboard

See previous blogs here.
And now for a smattering of interesting C. difficile associated publications since the last time I posted on this topic...
- An entire issue of the journal Anaerobe dedicated to C. difficile related issues is available here.
Notable articles in this journal include:- reviews of diagnostic testing
- probiotics (lack of efficacy in prevention and treatment according to the authors)
- fecal transplant (suggests that it does indeed work -- even if gross)
- the 'rixamixin chaser' (shows promise in multiple relapses, but not the magic bullet
- The potential role of an antitoxin (NEJM here)
- The development of disease in patients status post collectomy!
- The perils and difficulties of diagnosis.
- EIA sensitivity is relatively poor - ~60-70%
- GDH has better sensitivity, but poor specificity
- Cytotoxic assays are time consuming and expensive
- PCR may be less effort dependent but has an upfront cost
- An algorithm suggested is GDH as a screen, if positive confirm with EIA, if negative EIA do PCR or cytotoxic assay.
- A set of european guidelines, which seem quite reasonable.
- An article on the challenges of treating patients in the ICU including:
- lack of sensitivity of testing means potential undertreating of critically ill patients
- the role of vancomycin in severe disease
- the absence of diarrhea (as also reported from Toronto) in up to 20% of critically ill patients because of illeus, post-operative status, or narcotics
Wednesday, January 20, 2010
Candida Endopthalmitis
We've talked about candidemia before...
One of the complications of candidemia is the development of endogenous endopthalmitis. Different rates of occular involvement are quoted from 2%-40% depending on case series.
The majority of patients will develop endopthamitis within 2 weeks of candidemia. Particularly if there is a delay in treatment of the candidemia or if the candidemia is protracted.
One of the complications of candidemia is the development of endogenous endopthalmitis. Different rates of occular involvement are quoted from 2%-40% depending on case series.
The majority of patients will develop endopthamitis within 2 weeks of candidemia. Particularly if there is a delay in treatment of the candidemia or if the candidemia is protracted.
Early retinal exam can diagnosis, but follow up at 2 weeks is prudent as early lesions can be missed.
Treatment is covered in the IDSA guidelines (previously cited). Azole agents can be used for succeptible isolates. If there is a significant vitritis, sometimes vitrectomy with intraoccular amphotericin is required in addition to systemic therapy.
There are a number of good reviews here (treatment), here (case report and review of condition), here (BMJ review) and here (retinal lesions in sepsis, including description of occular manifestations).
Treatment is covered in the IDSA guidelines (previously cited). Azole agents can be used for succeptible isolates. If there is a significant vitritis, sometimes vitrectomy with intraoccular amphotericin is required in addition to systemic therapy.
There are a number of good reviews here (treatment), here (case report and review of condition), here (BMJ review) and here (retinal lesions in sepsis, including description of occular manifestations).
Tuesday, January 19, 2010
Klebsiella pneumoniae carbepenemase
We've talked a lot about this one -- but fortunately have yet to see one.
Some useful reviews/information:
Some useful reviews/information:
Monday, January 18, 2010
Cryoglobulinemia related to HCV
This weekend we saw a case of presumed cryoglobulemic vasculitis in a patient with known HCV. There is a previous blog related to HCV here, including a good link to a review on cryoglobulinemia. The following figure on causes of cryoglobulenemia is taken from said review:

Another review, particularly related to HCV is available here. In patients with HCV associated cryoglobulinemia, treatment of the HCV may be helpful in getting the condition under control.

Another review, particularly related to HCV is available here. In patients with HCV associated cryoglobulinemia, treatment of the HCV may be helpful in getting the condition under control.
Friday, January 15, 2010
Thursday, January 14, 2010
Histoplasmosis (actually was sporothrix!)
 Fascinating case today -- patient who works in construction who presented to hospital initially with hilar adenopathy, erythema nodosum and ankle arthritis who was initially diagnosed with sarcoidosis, but who went on to develop disseminated histoplasmosis with steroid therapy.
Fascinating case today -- patient who works in construction who presented to hospital initially with hilar adenopathy, erythema nodosum and ankle arthritis who was initially diagnosed with sarcoidosis, but who went on to develop disseminated histoplasmosis with steroid therapy.Histoplasmosis mimicing sarcoidosis with EN and arthritis has been described here and has been dubbed 'pseudosarcoidosis'. It has also been described here and here.
Several good reviews of histoplasmosis are available (here, and here- mainly pulmonary).
Manifestations include (but are not limited to):
- Asymptomatic -- majority!
- Acute pulmonary histoplasmosis
- Usually self-limited febrile illness with respiratory symptoms. Mediastinal lymphadenopathy common. Can have erythema nodosum and be mistaken for sarcoidosis.
- Mild forms do not require treatment.
- Chronic cavitary pulmonary histoplasmosis
- Granulomatous mediastinitis
- large necrotic mediastinal nodes cause compressive symptoms
- large necrotic mediastinal nodes cause compressive symptoms
- Fibrosing mediastinitis
- Pericarditis
- Disseminated (Systemic) Disease
- Ususally immunosuppressed patients: AIDS (CD4 below 150), hematologic malignancies, transplant patients, steroids, TNF alpha inhibitors, congenital immunodeficiencies
- May occur during initial infection or as reactivation event years later
- Every organ system may be involved. Commonly, fever, arthralgias, anorexia, malaise. Pancytopenia, hepatosplenomegaly. GI involvement with diarrhea common.
- Endocardtitis/endovascular
- CNS disease
Addendum:
- Even more interesting -- the case turns out to be sporothrix schenckii instead of histoplasma!
- See description of sporothrix mimicking sarcoid here, and IDSA guidelines for sporothrix here. There are no published cases like ours to date -- expect that to change.
- According to this article -- Amphotericin B and itraconazole are the most active. Voriconazole is not active, nor is fluconazole.
Wednesday, January 13, 2010
Bilateral leg 'cellulitis'
A number of consults for this clinical entity today makes me want to provide you with this excelllent review of the mimickers of cellulitils.... The most common mimicker I see is venous stasis dermatitis, often bilateral, in the obese patient with heart failure.
Tuesday, January 12, 2010
Peripartum sepsis with Group A Streptococcus
Today we saw a case of group A streptococcal bacteremia associated with peripartum sepsis and intrabdominal abscesses. This is similar to a case reviewed here (and here). NEJM case report here.
The case definition (epidemiologic) for streptococcal toxic shock syndrome (CDC) includes:
Treatment includes supportive care, debridement of necrotic/non-viable tissues and source control , consideration of IVIG , and antibiotic therapy with beta-lactam (i.e. penicillin) with clindamycin (for its anti-ribosomal activity and effect on non-log phase growth); however, recent data suggests that exotoxin production may actually be increased if the organism is clindamycin resistant. Linezolid may be an alternative anti-ribosomal agent in this case.
The case definition (epidemiologic) for streptococcal toxic shock syndrome (CDC) includes:
- hypotension defined by a systolic blood pressure less than or equal to 90 mm Hg for adults
- Multi-organ involvement characterized by two or more of the following:
- Renal impairment: Creatinine greater than or equal to 2 mg/dL (greater than or equal to 177 µmol/L) for adults. In patients with preexisting renal disease, a greater than twofold elevation over the baseline level.
- Coagulopathy: Platelets less than or equal to 100,000/mm3 (less than or equal to 100 x 106/L) or disseminated intravascular coagulation, defined by prolonged clotting times, low fibrinogen level, and the presence of fibrin degradation products.
- Liver involvement: Alanine aminotransferase, aspartate aminotransferase, or total bilirubin levels greater than or equal to twice the upper limit of normal for the patient's age. In patients with preexisting liver disease, a greater than twofold increase over the baseline level.
- Acute respiratory distress syndrome: defined by acute onset of diffuse pulmonary infiltrates and hypoxemia in the absence of cardiac failure or by evidence of diffuse capillary leak manifested by acute onset of generalized edema, or pleural or peritoneal effusions with hypoalbuminemia.
- A generalized erythematous macular rash that may desquamate.
- Soft-tissue necrosis, including necrotizing fasciitis or myositis, or gangrene.
Treatment includes supportive care, debridement of necrotic/non-viable tissues and source control , consideration of IVIG , and antibiotic therapy with beta-lactam (i.e. penicillin) with clindamycin (for its anti-ribosomal activity and effect on non-log phase growth); however, recent data suggests that exotoxin production may actually be increased if the organism is clindamycin resistant. Linezolid may be an alternative anti-ribosomal agent in this case.
Friday, January 8, 2010
Candidemia redux
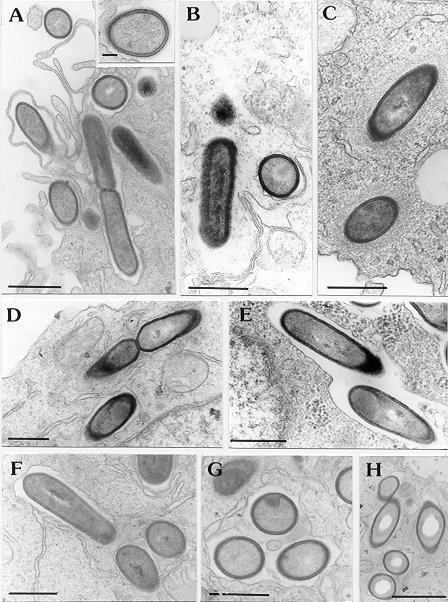
See previous blog. Today we saw a patient with candidemia, presumably from a urinary source. We discussed species identification, and the use of the germ tube test for rapid identification of Candida albicans.
This article discusses the clinical utility of the germ tube test, quoting a sensitivity of 87% and specificity of 100% for identifing C. albicans -- directly off of the positive blood culture! This saves ~24h in the rapid identification of C. albicans, as the germ tube is traditionally performed off a subculture on fungal medium, adding up to a 24h delay.
This article discusses the clinical utility of the germ tube test, quoting a sensitivity of 87% and specificity of 100% for identifing C. albicans -- directly off of the positive blood culture! This saves ~24h in the rapid identification of C. albicans, as the germ tube is traditionally performed off a subculture on fungal medium, adding up to a 24h delay.
Thursday, January 7, 2010
Strongyloides
 Previously mentioned 'strongy' here. CMAJ reviews here, and here.
Previously mentioned 'strongy' here. CMAJ reviews here, and here.There was an extensive discussion at case-rounds yesterday afternoon about prophylaxis for strongyloidiasis in patients at risk who will be immunosuppressed.
Here is a review of strongyloidiasis in the immunocomprimised patient.
This article discusses prevention in patients with connective tissue diseases.
In patients with bone marrow transplantation or solid organ transplantation recent guidelines suggest that patients with unexplained eosinophilia or who have lived/travelled in areas endemic for strongyloidiasis, even if remotely, should be screened prior to transplant with stool O&P time three and serology. Positive screening or eosinophilia should prompt pre-emptive treatment prior to transplant with ivermectin. Mind you, some experts would suggest, given the few side effects, that people who have lived in endemic areas should just be treated...
Recent case report of death due to strongyloides in patient with HSCT...
Wednesday, January 6, 2010
TB - Tuberculosis Hodge-podge
Yesterday we saw an interesting case at the end of the day of a patient on immunosuppression who presented with a new left sided pleural effusion and some parenchymal changes compatible with a flare of her underlying lung disease vs. tuberculosis.
This patient comes from an endemic country and has evidence of fibronodular changes on chest x-ray (RR for reactivation ~15). There has been no previous TB treatment.
This highlights a large number of good teaching points:
- Diagnosis and management of latent TB.
- Diagnostic approach to possible TB pleuritis.
- The interplay between TB and TNF-alpha inhibitors.
- The radiographic manifestations of TB and the differences in immunosuppressed hosts.
- The yield of bronchoscopy in patients who are not coughing.
- The potential role for gastric aspirate to make the diagnosis
FYI - Canadian Tuberculosis Standards (Guidelines) available for free here.
Tuesday, January 5, 2010
Streptococcus milleri group
Today we reviewed a case of multiple soft tissue abscesses caused by an organism of the Streptococcus milleri group.
This group of organisms includes:
- S. anginosus
- S. intermedius
- S. constellatus
Because of phenotypic similarities, exact speciation can be difficult without more advanced means of testing. Speciation matters as intermedius and constellatus are very frequently associated with abscess formation; wheras anginosis is not. The clinical presentations of the various species are discussed in this CID article. Soft tissue abscesses are most common, followed by pleuropulmonary (including empyema), intrabdominal (including liver abscess), and brain abscesses.
The propensity to form abscesses may be related to impaired neutrophil chemotaxis and resistance to destruction when phagocytosed.
Treatment involves adequate surgical source control, and antibiotics, usually parenteral beta-lactams such as Penicillin G if the isolate is susceptible. Duration of therapy varies depending on location of abscess and adequacy of surgical drainage.
Monday, January 4, 2010
Staphylococcal bacteremia
Am back on clinical service today! So, I will begin to blog again...
Today we discussed Staphylococcus aureus bacteremia including MRSA. I have previously blogged about this here -- with links to what I believe are the relevant articles.
I will add this article from CID which discusses combination antibiotic therapy in MRSA infections.
Today we discussed Staphylococcus aureus bacteremia including MRSA. I have previously blogged about this here -- with links to what I believe are the relevant articles.
I will add this article from CID which discusses combination antibiotic therapy in MRSA infections.
Subscribe to:
Posts (Atom)