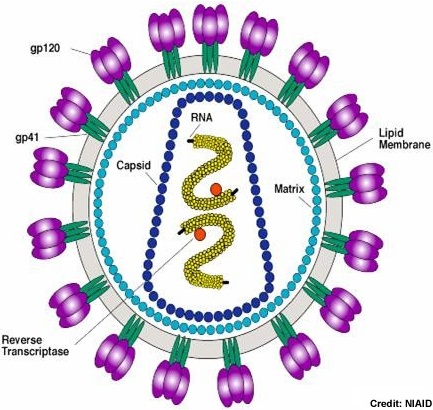
Today I facilitated morning report where the presented a case of encephalopathy in a patient with advanced HIV. There was a good possibility this was related to HIV encephalopathy assuming cryptococcal meningitis (prev blog) was ruled out. I have previously blogged about acute confusional states here including links to discussions on paraneoplastic syndromes.
This is a recent review of HIV and its neurologic sequelae. Another review is available here. A more focussed review on HIV encephalopathy including treatment options is available here.
This is a helpful article on the neuroradiology of HIV related CNS processes.
(I'm not providing you with medical advice. Clinical correlation and professional interpretation required)
Monday, August 24, 2009
Wednesday, August 19, 2009
From the Conference: Notable papers in treatment of mucormycosis
As referenced by Dr. Rotstein:
Epidemiology in Transplant patients (link)
Epidemiology in All patients (link)
Clinical trial low vs. high dose AmB (link)
Review of management of mucormycosis (link)
Combination polyene and echinocandin evidence (link)
Not referenced by Dr. Rotstein, but I find it interesting:
Risk of death without initial AmB therapy for invasive mould infections (link)
Epidemiology in Transplant patients (link)
Epidemiology in All patients (link)
Clinical trial low vs. high dose AmB (link)
Review of management of mucormycosis (link)
Combination polyene and echinocandin evidence (link)
Not referenced by Dr. Rotstein, but I find it interesting:
Risk of death without initial AmB therapy for invasive mould infections (link)
Tuesday, August 18, 2009
From the Conference: Hot Topics in HIV
As presented by Sharon Walmsley:
- "When to start"
At diagnosis? Treatment as prevention- Sullivan P et al., 16th CROI Montreal, Feb 2009: 3,000 discordant couples no ARV vs. partner on treatment -- dramatically reduced risk of linked infections 3.4/100 vs. 0.7/100 person years
Viral load - higher?
Co-morbid illness
Initiate at dx vs. CD4:- Fitzgerald D, et. al, 5th IAS: Cape Town, South Africa July 19-22, Abst. WESY201 stopped due to excess death in delayed arm
- Kitahata M, et al: Cohort study: individuals who deferred HAART to below CD4 500 were at increased risk of progression.
- Sterne J et al., 16th CROI Montreal Feb 2009: Cohort study: advantage to starting earlier in terms of risk of AIDS or death regardless of CD4 count
- "Inflammation is BAD"
DAD Study:- Friis-Moller N et al, CROI 2006: Are ARVs associated with increased cardiovascular events? PIs associated with increased risk of CVD above risk of dyslipidemia.
- Baseline MI risk 1.6%, 1.9x more ABC, 1.6 more PI, 3x more smoking
- Associated editorial by Friis-Moller here
- Baseline MI risk 1.6%, 1.9x more ABC, 1.6 more PI, 3x more smoking
- Sabin C et al., CROI 2008; Lundgren JD et al, CROI 2009: Increased risk with ABC, ddI, lopinavir
- Lang S et al, 16th CROI: ABC exposure within 6 months was associated with slight increase in MI risk, also lopinavir and indinavir
- GSK and VA study to not find similar ABC risk
- Do planned structured treatment interruptions benefit patients? No -- there was increased risk of CV death and death from OI
- Friis-Moller N et al, CROI 2006: Are ARVs associated with increased cardiovascular events? PIs associated with increased risk of CVD above risk of dyslipidemia.
- Antiretroviral monotherapy - Has it come of age?
AZT inferior to AZT+3TC inferior to AZT+3TC+PI/NNRTI
But what about newer single agent:- LPV/r monotherapy (example publication of this data here):
- Either as initial therapy, with NRTI backbone then stop, with any regimen that supresses then change to monotherapy
- MONOI Study (Katlama, IAS 2009 Abstract) - Darunavir/ritonavir as monotherapy:
- Suppress then monotherapy vs. continue -- 94% virologic success with DRV/r monotherapy at 48 weeks vs. 99% with DRV/r +NRTIs. Failed to meet pre-specified inferiority
- MONET Study (J. Arribas et al, IAS, Cape Town July 2009)
- Non-inferiory of monotherapy to with NTRIs -- 84.3% vs. 85.3% @ 48 weeks
- LPV/r monotherapy (example publication of this data here):
- "Mother to child transmission - has it been eliminated?"
Risk is currently less than 1% with antenatal testing, antenatal ARV to VL below 50, selective elective C-section, neonatal ART and avoidance of breast feeding- Does C-section add anything to HAART? Yes, if not on ART or VL not less than 50
- Treat mother or newborn? Shapiro R, et. al 5th IAS Cape Town/Chasela C. et al, 5th IAS
- If you treat the mothers, get them undetectable, than even with breast feeding transmission can be less than 1% -- of potential great benefit in the developing world
- "New Drugs"
- Goal is VL less than 50 regardless of naive or experienced with regimens of 2-3 active drugs from different classes
- Will initial regimens change?
- Entry inhibitors (CCR5 blocker - requires tropism assay) - miraviroc
- Integrase inhibitor - raltegravir, elvitegravir
- Maturation inhibitor - bevirimat
- New agents, old classes: etravirine, rilpilvarine (NNRTI), tipranavir, darunavir (PI)
From the Conference: Hot Papers in ID
As presented by Matthew Muller (in order of presentation):
- "The Animal Rule" - Raxibacumab for the Treatment of Inhalational Anthrax
- "The Acid Truth" - Acid suppressive medication use and the risk of hospital-acquired pneumonia
- "If it ain't Dutch, it ain't much" - Decontamination of the Digestive Tract and Oropharynx in the ICU
- "Zero Tolerance for CLI" - Chlorhexadine-Impregnated Sponges and Less Frequent Dressing Changes for Prevention of Catheter-Related Infections in Critically ill Adults: a Randomized Controlled Trial
- "Short Red Snappers" - Adverse Events with 4 months of Rifampin therapy or 9 months of isoniazid therapy for latent TB
- "Short Red Snappers (2)" - Moxifloxacin vs. Ethambutol in the initial treatment of tuberculosis: a double-blind, randomized, controlled phase II study
- "Maybe yes, maybe no" - Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. Accompanying editorial here.
- "Pandemic Influenza - Much ado about nothing?" - Severe Respiratory Disease Concurrent with the circulation of H1N1
Thursday, August 13, 2009
Septic Thrombophlebitis
Not surprisingly, this clinical entity is similar in many ways to both deep vein thrombosis and bacteremia.
Most common sites include: pelvis in association with C-section, IJ in association with infections of head/neck, portal vein related to intrabdominal infections such as diverticulitis or appendicitis, and the veins of the upper limbs in association with indwelling central catheters
Treatment involves medical therapy with intravenous antibiotics and often heparin (review here). Surgical intervention or thrombolysis are reserved for refractory cases. Treatment duration variable.
This article reviews Lemierre's syndrome (also see orignial article from 1936) -- Septic thrombophlebitis of the internal jugular vein with associated Fusobacterium necrophorum septicemia and metastatic infection.
Most common sites include: pelvis in association with C-section, IJ in association with infections of head/neck, portal vein related to intrabdominal infections such as diverticulitis or appendicitis, and the veins of the upper limbs in association with indwelling central catheters
Treatment involves medical therapy with intravenous antibiotics and often heparin (review here). Surgical intervention or thrombolysis are reserved for refractory cases. Treatment duration variable.
- In uncomplicated cases, with limited superficial vein involvement, and negative blood cultures, treatment can be as short as 48h past clinical stability, normalization of the white count, and defervessence.
- In other cases with bacteremia and/or metastatic spread treatment duration will range 2-6 weeks.
This article reviews Lemierre's syndrome (also see orignial article from 1936) -- Septic thrombophlebitis of the internal jugular vein with associated Fusobacterium necrophorum septicemia and metastatic infection.
Wednesday, August 12, 2009
Brain abscess

The cleverly drawn figure above demonstrates the principle mechanisms by which people develop a brain abscess. The mechanism of acquisition of the brain abscess has direct bearing on the likely organisms. The most common mechanism is by spread from the adjacent sinuses or oral cavity making the most common organisms in the immunocompetent:
- Oral streptococci (viridans group, milleri group)
- Staphylococcus aureus
- Oral anaerobes including peptostreptococcus, bacteroides and fusobacterium species
The "heart" in the diagram includes:
- Hematogenous spread in bacteremia such as seen in the lung/brain or liver/brain axis
- Right to left shunting in HHT or cyanotic heart disease or other AV malformations
- Infective endocarditis
Tuesday, August 11, 2009
Fever and Polyarthritis
Review article here from NEJM
Consider the following most common etiologies:
Consider the following most common etiologies:
- Infectious:
- Bacterial Infection of Joints
- Staphylococcus aureus
- Group G Streptococcus
- Neisseria gonorrrhoeoe and meningiditis
- Bacterial Endocarditis
- Lyme disease
- Secondary Syphilis (usually with rash)
- Mycobacteria/Fungal
- Viral
- Parvovirus B19
- Rubella
- HIV seroconversion
- Hepatitis B and C
- Parvovirus B19
- Bacterial Infection of Joints
- Post-Infectious
- Reactive arthritis post Chlamydia or enteric infection
- Rheumatic Fever or Post-Streptococcal Arthritis
- Rheumatologic
- Rheumatoid Arthritis
- Lupus
- Systemic Vasculitis (i.e. PAN)
- Still's Disease
- Crystal Induced Arthritis
- Other (i.e. IBD associated arthritis)
Monday, August 10, 2009
Ventlator Associated Pneumonia (VAP)
Good reviews are available here and here.
Diagnosis:
10-20% of patients receiving mechanical ventilation for more than 48 hours will develop VAP
Some controversy exists about how to precisely define the diagnosis. However in general if you have a new or worsening CXR infiltrate with two or more of:

A score of greater than or equal to 6 is suggestive of VAP. You should obtain samples from the LOWER respiratory tract -- not ET aspirates. There is a study suggesting ET aspirate is acceptable, but patients with Pseudomonas and MRSA were excluded as were many other patients. Samples may be obtained from either direct visualization with BAL or blind BAL, ideally before antibiotics, but antibiotics should not be significantly delayed.
Prevention:
Diagnosis:
10-20% of patients receiving mechanical ventilation for more than 48 hours will develop VAP
Some controversy exists about how to precisely define the diagnosis. However in general if you have a new or worsening CXR infiltrate with two or more of:
- Fever or hypothermia
- Sputum production
- Increased WBC count

A score of greater than or equal to 6 is suggestive of VAP. You should obtain samples from the LOWER respiratory tract -- not ET aspirates. There is a study suggesting ET aspirate is acceptable, but patients with Pseudomonas and MRSA were excluded as were many other patients. Samples may be obtained from either direct visualization with BAL or blind BAL, ideally before antibiotics, but antibiotics should not be significantly delayed.
Prevention:
- elevation of the head of the bed
- daily sedation vacations or even awake ventilation
- assessment of readiness to extubate
- "if you never re-intubate any patients, you are not extubating soon enough"
- "if you never re-intubate any patients, you are not extubating soon enough"
- peptic ulcer disease prophylaxis
- deep venous thrombosis prophylaxis
- orogastric feeding as opposed to nasogastric
- use of feeds in general is associated with less colonization
- Initiate good empiric therapy based on local hospital epidemiology
- Piperacillin-Tazobactam PLUS ciprofloxacin is suggested @ our site
- Vancomycin if high suspicion for MRSA
- NB: The vancomycin vs. linezolid debate discussed here
- NB: The vancomycin vs. linezolid debate discussed here
- De-escalate approrpiately -- Tailor to cultures, CPIS less than 6 @ 72h consider early discontinuation

- Duration: Treat for 8 days if clinically improved, CPIS less than 6, 15 days if not improved or if Pseudomonas or MRSA (JAMA trial here)
Thursday, August 6, 2009
Klebsiella Liver Abscess
 See previous liver abscess blog
See previous liver abscess blogThese articles describe a syndrome of klebsiella liver abscess caused by a so-called hypermucoviscous strain that presents with liver abscess and metastatic complications including CNS infection, endopthalmitis, septic pulmonary emboli, and pericarditis.
Wednesday, August 5, 2009
Fever in the Retuned Traveller
 This was technically yesterday's case -- but since we only had one case today I thought this would be a better topic for the blog.
This was technically yesterday's case -- but since we only had one case today I thought this would be a better topic for the blog.Two excellent reviews of the spectum of illnesses causing fever in the returned traveller are available from CID here and the NEJM here.
Keys in history:
- What pre-travel preparation (vaccines, prophylaxis) was received? Was it taken? How many doses were missed?
- Where did they go (as exact as possible)? What were the exact dates and places?
- When did they return?
- When did they get sick?
- What exposures did they potentially have?
- Food
- Water (drinking/swimming)
- Animals (including humans -- i.e. sexual contacts, blood exposure, sick contacts)
- Vectors (mosquitos, ticks, other)
- What, if any, localizing features do they have on history or physical exam?


A recent publication using the same database suggests that of the diarrheal illnesses, parasitic infections are most common, followed by campylobacter, shigella and salmonella.
Tuesday, August 4, 2009
Varicella (Herpes) Zoster Redux
Today we saw a case of multidermitomal shingles with V1 disease and associated VZV keratitis. See previous blog on shingles here.
Additional interesting zoster related articles:
Additional interesting zoster related articles:
- Recent JAMA clinical cross-roads, including discussion on post-herpetic neuralgia.
- Mayo Clinic Proceedings Review with good table on PHN.
- Case reports of disseminated zoster in patients with HIV despite good CD4 counts
- Good review of acute retinal necrosis (ARN) and treatment thereof
Friday, July 31, 2009
Lyme Disease
 Review here and NEJM reviews here and here. IDSA 2006 guidelines on tick borne illness here.
Review here and NEJM reviews here and here. IDSA 2006 guidelines on tick borne illness here.Transmitted by ticks of the Ixodes family, usually nymphs (see photos), this spirochete infection causes the following recognized syndromes:
- Early localized infection: characteristic rash (erythema chronica migrans) with cleared centre, of at least 5cm diameter, in context of possible fever, chills, headache, malaise, myalgias.
- Early disseminated infection: few days to weeks post infection. Additional ECM lesions in presence of musculoskeletal symptoms (60% - i.e. migratory arthritis, muscle and joint pain), neurological (15% -- i.e. facial nerve palsy, menigoencephalitis, radiculopathies) or cardiac (10% -- i.e. AV block)
- Late disseminated infection: up to 60% untreated. Arthritis of knees and hips, occasionally a slowly progressive encephalopathy or polyradiculopathy.
Recent article on the emergence of this disease in Canada. This article has probably caused more phone calls to the ID service for 'Lyme' in the past few months than in the past few years. The article demonstrates the expansion of the territory of the Ixodes tick and the concern is that where the tick goes, the pathogen will eventually follow.

 Treatment for early disease is oral doxycycline (or amoxicillin in patients whom doxycycline is contraindicated) for 14-21 days. EDIT: 10 days is sufficient
Treatment for early disease is oral doxycycline (or amoxicillin in patients whom doxycycline is contraindicated) for 14-21 days. EDIT: 10 days is sufficientRemember: to get Lyme disease you need to be bitten by the right tick (see below), at the right time of year, in the right place in the world. The majority of consults seen outside endemic areas (or travel to) involve the wrong tick and the wrong place. In these cases Lyme serology will *not* be helpful due to the low specificity.
NB: NEJM review of 'chronic lyme disease' that is worth a read....

I found this site useful as well...
Addendum -- Death from chronic lyme treatment...
Thursday, July 30, 2009
Latent Tuberculosis
From the Canadian TB standards:
Who to test for LTBI?
 False negative:
False negative:
Treatment:
NNT~10 for reactivation in the general population. Risk reduction from ~10% to 1% lifetime of reactivation. Lower NNT in at-risk groups.
Who to test for LTBI?
- Contacts of a known case
- Immigrants to Canada within the past 2 years
- Healthcare workers or those at high risk of nosocomial exposure
- Immunosuppressed patients (HIV, transplant, high dose steroids, TNF-alpha, etc.)
- Radiographic evidence of possible old TB without symptoms and no diagnosis
- Mantoux test (PPD) 5-TU intradermal injection
- Read at 48-72 hours
- Record the number of millimetres of induration (raised area, not just red) without rounding

 False negative:
False negative:- Severe illness including active TB
- Malnutrition
- Immunosuppression (iatrogenic, HIV, etc)
- Major viral illness
Treatment:
- Exclude active disease
- INH 300mg PO OD x 9 months +/- Vitamin B6 25mg PO OD
OR
RIFAMPIN 600mg PO OD x 4 months
NNT~10 for reactivation in the general population. Risk reduction from ~10% to 1% lifetime of reactivation. Lower NNT in at-risk groups.

Wednesday, July 29, 2009
C. difficile

Previous blog here.
Some more "novel stuff":
- Case reports (poor quality really) of the use of tigecycline for the treatment of severe CDAD.
- Article discussing the use of the non-absorbable rifamycin, rifaximin, for the treatment of CDAD -- AKA the "rifaximin chaser"
Tuesday, July 28, 2009
Stenotrophomonas maltophilia
 Today we saw a patient with S. maltophilia catheter related bacteremia.
Today we saw a patient with S. maltophilia catheter related bacteremia.Review of the microbiology of this organism here.
- Straight or slightly curved, motile gram negative rod
- Obligate aerobe, will grow best at 35 degrees
- Non-lactose fermenter, catalase positive, oxidase negative
- Will grow on blood agar and MacConkey -- and can be selected for using imipenem innoculated plates as they are carbepenem resistant organisms.
- Prior antibiotic therapy
- Central venous catheters
- Neutropenia or cytotoxic chemotherapy
- ICU/Mechanical ventillation/Tracheostomy
- Malignancy or steroid use
Distinguishing between colonization and infection can be difficult, particularly for respiratory isolates. Bacteremia is a common presentation with an attributable mortality of up to 60%. ICU admission (APACHE more than 15), shock and thrombocytopenia are associated with mortality.
Endocarditis can occur, as can hospital acquired pneumonia, nosocomial meningitis, cellulitis and urinary tract infection.
TMP-SMX is the antimicrobial agent of choice (greater than 90% are sensitive). Combination with ticarcillin/clavulanate should be considered for serious infections. Quinolones may be a reasonable alternative in the TMP/SMX resistant or intolerant but consideration should also be given to combining them with ticarcillin/clavulinate.

Monday, July 27, 2009
Nodular Lymphangitis
 This weekend we saw a case of nodular lymphangitis presenting with a chronic draining infection of the hand and ascending nodular lymphangitis. This was in the context of significant animal exposures and fish tank exposures.
This weekend we saw a case of nodular lymphangitis presenting with a chronic draining infection of the hand and ascending nodular lymphangitis. This was in the context of significant animal exposures and fish tank exposures.

Friday, July 24, 2009
Acute Respiratory Distress Syndrome
Today we saw a case of a patient with subacute progressive hypoxemic respiratory failure for which no infectious etiology could be confirmed.
Many different pathogens can cause sepsis, which in turn can be associated with ARDS. In terms of specific pathogens, the following are reported to cause ARDS (outside of the usual pneumonia --> sepsis --> ARDS):
Guidelines for the management of severe sepsis (including ARDS) are available here.
Many different pathogens can cause sepsis, which in turn can be associated with ARDS. In terms of specific pathogens, the following are reported to cause ARDS (outside of the usual pneumonia --> sepsis --> ARDS):
- Bacterial
- S. pneumoniae
- Gram negative rods including Pseudomonas
- Legionella, Chlamydophilia, Mycoplasma
- Tuberculosis
- Viral
- Influenza A (and B) particularly H5N1 but also H1N1 and seasonal
- Coronavirus (SARS)
- Varicella Zoster (in primary infections)
- Influenza A (and B) particularly H5N1 but also H1N1 and seasonal
- Parasite
- Plasmodium Falciparum
Guidelines for the management of severe sepsis (including ARDS) are available here.
Thursday, July 23, 2009
Foley Catheter Related Urinary Tract Infection
Its not sexy -- but we saw a case of foley catheter related urinary tract infection. These two articles discuss this phenomenon (#1 #2)
The risk is approximately 5% per day of insertion and strategies aimed at minimizing this infection (as article above) are important to reduce cost, morbidity and mortality.
The risk is approximately 5% per day of insertion and strategies aimed at minimizing this infection (as article above) are important to reduce cost, morbidity and mortality.
Wednesday, July 22, 2009
Tuesday, July 21, 2009
Group B Streptoccal Bacteremia
 Reviews here and here.
Reviews here and here.Also known as Streptococcus agalactiae, group B streptococcus is a pathogen that causes a variety of infectious syndromes. It colonizes the human GI tract and causes infection usually through a breach of the epithelial barriers.
In pregnant women it can cause choramnionitis and post-partum endometritis. In the neonate, it is a significant cause of neonatal sepsis and meningitis and this is why women are screened for carriage and given peri-partum antibiotics.
In the non-pregnant adult, it is commonly associated with:
- Bacteremia without focus (~40-50%)
- Skin/soft tissue infections (~20%)
- Pneumonia (~10-15%)
- Osteomyeltis or Septic Arthtitis (~10-15%)
- Other (Endocarditis, Peritonitis, Meningitis)
Treatment includes a beta-lactam antibiotic (vancomycin in the penicillin allergic) pending sensitivities to other agents like the quinolones or clindamycin. GBS is universally penicillin sensitive at present. Source control is also important.
Monday, July 20, 2009
Staphylococcus Aureus Bacteremia
 I direct you to previous posts here and here which discuss this entity. My often quoted articles including the ones on prognosis are available there. A new article on complications is available here.
I direct you to previous posts here and here which discuss this entity. My often quoted articles including the ones on prognosis are available there. A new article on complications is available here.This is a new review, which seems to be useful.
This article discusses the challenges of MRSA bacteremia. The challenges of MRSA are also covered here.
Friday, July 17, 2009
Adult Epiglotitis
 Reviews here, here and JAMA case series here.
Reviews here, here and JAMA case series here.While the introduction of the Haemophilus influenzae type B vaccine has reduced the incidence in children, acute epiglotitis continues to occur in adults.
Patients present with sore throat, odynophagia , fever, dyspnea, drooling, dysphagia, foreign body sensation, and stridor.
Diagnosis can be made on the lateral neck radiograph (thumb-print sign) or on direct fiberoptic laryngoscopy.
The most common pathogens are oral flora including non-typable haemophilus species and group A streptococci. Treatment includes a third generation cephalosporin in association with close monitoring and airway management. Steroids (dexamethasone) are commonly used to decrease swelling, but the evidence for their use is actually limited.
About 40-50% will need invasive airway management (intubation, tracheostomy)
Thursday, July 16, 2009
Wednesday, July 15, 2009
Diabetic Foot
Tuesday, July 14, 2009
Dog Bite Infection

Good review on dog and cat bite infections here.


Prophylaxis: Amoxicillin-clavulinate or in penicillin allergic doxycycline + metronidazole (or clindamycin and moxifloxacin/levofloxacin).
Treatment of infection: Will require admission, surgical debridement with culture and broad spectrum antibiotics with gram negative and anerobic coverage (i.e. piperacillin-tazobactam, carbepenems, 3rd generation cephalosporin with metronidazole)
Pasturella multilocida, a gram-negative bacilli, is resistant to cephalexin and clindamycin. It is oxidase positve, indole positive, and won't grow well on MacConkey agar.
Capnocytophagia canismorsis, another fastidious gram negative rod is also oxidase and catalase positive. In patients with underlying immunodeficiency (splenectomy, cirrhosis, hypogammaglobulinemia) infections can progress to florid septic shock with multiorgan failure and DIC. It is hard to grow in the laboratory, and treatment should start early.
Monday, July 13, 2009
Vertebral Osteomyelitis
There is a review of osteomyelitis here with some images which I found useful below.

 Because of the variety of causative organisms involved, a tissue diagnosis through bone biopsy is preferable to empiric treatment.
Because of the variety of causative organisms involved, a tissue diagnosis through bone biopsy is preferable to empiric treatment.
This article describes candidal vertebral osteomyelitis, which is also common in the IDU population and requires extended courses of treatment.

 Because of the variety of causative organisms involved, a tissue diagnosis through bone biopsy is preferable to empiric treatment.
Because of the variety of causative organisms involved, a tissue diagnosis through bone biopsy is preferable to empiric treatment.This article describes candidal vertebral osteomyelitis, which is also common in the IDU population and requires extended courses of treatment.
Friday, July 10, 2009
Necrotizing Fasciitis
 Today we saw a case of necrotizing skin and soft tissue infection (not quite necrotizing fascitis) presenting in the groin area of a diabetic patient.
Today we saw a case of necrotizing skin and soft tissue infection (not quite necrotizing fascitis) presenting in the groin area of a diabetic patient.Patients who inject drugs or who have diabetes, obesity, or immunosuppression are at higher risk of these infections. Pain is an early presenting feature with later development of haemodynamic instability. Early changes resemble cellulitis; however, late changes include tense edema outside the area of compromised skin, pain disproportionate to appearance, skin discoloration, blisters/bullae and necrosis, and crepitus and/or subcutaneous gas.


Necrotizing fascitis (review) can be characterized based on the pathogens involved:
- Type I: Mixed aerobic and anaerobic infection. Often in diabetics. Includes Fornier's gangrene where the infection involves the fascial planes in the perineal area and in males can involve the scrotum and penis.
- Type II: Group A Streptococcus and MRSA
- Other organisms (below)
 Treatment:
Treatment:- Highly skilled surgical debridement and source control
- Appropriate antibiotics (in GAS penicillin G and clindamycin for Type I broad spectrum anaerobic and gram negative coverage -- i.e. piperacillin-tazobactam)
- IVIG -the case-control study on the use of IVIG in Invasive Group A Streptococcal disease is available here.
- Treatment of close contacts discussed here.
Thursday, July 9, 2009
Endocarditis
We discussed endocarditis today. I will take this opportunity to 'show off' the search function of the blog and direct you here.
Duke Criteria:
Major Criteria
Microbiologic:
Positive blood cultures (>=2) with an organism that classically causes endocarditis (viridans group streptococci, staphylococcus aureus, enterococcus, HACEK organisms)
OR
Persistantly positive (>=3 or >=2 12h apart) for another organism
Echocardiologic:
Vegetation on valve not otherwise explainable or dehiscence of mechanical valve or abscess
OR
Clinical: *NEW* (not worsening) regurgitant murmur
Minor Criteria
The ACC has updated guidelines on the management of valvular heart disease including endocarditis and endocarditis prophylaxis. These address the diagnostic algorithm and treatment in more detail.
Duke Criteria:
Major Criteria
Microbiologic:
Positive blood cultures (>=2) with an organism that classically causes endocarditis (viridans group streptococci, staphylococcus aureus, enterococcus, HACEK organisms)
OR
Persistantly positive (>=3 or >=2 12h apart) for another organism
Echocardiologic:
Vegetation on valve not otherwise explainable or dehiscence of mechanical valve or abscess
OR
Clinical: *NEW* (not worsening) regurgitant murmur
Minor Criteria
- Predisposition -- known pre-existing valvular disease or IVDU
- Fever
- Evidence of vascular phenomenon -- septic emboli, mycotic aneurysm, Janeway lesions,
- Immunologic: glomerulonephritis (like this case), positive RF, roth spots, Osler nodes,
- Microbiologic: Blood culture not meeting major
- Echocardiographic not meeting major
The ACC has updated guidelines on the management of valvular heart disease including endocarditis and endocarditis prophylaxis. These address the diagnostic algorithm and treatment in more detail.
Tuesday, July 7, 2009
Prosthetic Joint Infection
Today we discussed prosthetic joint infection (Recent review here)
UPDATE AUG 20 - NEJM Review Recently Published here.

Treatment options include:
Also -- here is a review of the use of combination rifampin with other antibiotics for the treatment of Staphyloccal infections.
UPDATE AUG 20 - NEJM Review Recently Published here.

Treatment options include:
- 2 stage revision -- removal of hardware, insertion of spacer with ~6weeks antibiotics before re-implantation. Highest chance for cure, significant morbidity
- 1 stage revision -- removal of hardware, debridement and re-implanataion with concomitant antibiotics. Less morbidiy, less chance of cure
- Debridement, Antibiotics and Retention -- chance of failure, little morbidity
- Palliation -- i.e. chronic suppressive antibiotics
- Relatively short duration of illness
- No loosening of the prosthesis
- Healthy overlying tissues
- Full OR debridement occurs
- The organism is susceptible to quinolones and rifampin (and the patient can tolerate both)
Also -- here is a review of the use of combination rifampin with other antibiotics for the treatment of Staphyloccal infections.
Monday, July 6, 2009
Severe Falciparum Malaria

We discussed a case of a patient with 3% parasitemia but who had CNS symptoms compatible with cerebral malaria and mild renal failure.
In general, severe malaria is defined as a parasitemia of greater than 5% or disease associated with end-organ dysfuction (see NEJM article and table below)

We also discussed the use of artesunate in the treatment of malaria. This Cochrane review suggests that as compared with IV quinine, artesunate reduced the risk of death (RR 0.62), cleared parasitemia faster, and had a lower risk of hypoglycemia. Consequently, it is likely currently the therapy of choice for severe malaria in non-pregnant adults.
Dosing is 2.4mg/kg given as an IV push at time 0, 12h, 24h and 48h. It is given in combination with a longer acting antimalarial such as doxycycline 100mg PO BID x 7days.
Generally fewer side effects than quinine or quinadine. Side effects include:
- GI symptoms (relatively common)
- Allergy ~1:3000
- Possible neurotoxicity manifesting as oto/vestibular toxicity (rare)
Friday, July 3, 2009
Candidemia
Today we discussed candidemia. The 2009 IDSA guidelines are available here.
In general:
In general:
- If the patient is critically ill, has recently been exposed to azoles, or the local prevalence of azole resistant candida is high initial therapy should be an echinocandin. Otherwise an azole like fluconazole would be appropriate.
- Line foci *must* be removed
- You should look for metastatic spread including the eyes or heart valves. Other investigations to look for osteomyelitis or septic thrombophlebitis should be based on history and clinical suspicion.
- Treatment duration varies depending on complication. In general, if there is no evidence of metastatic spread of infection treatment duration is 2 weeks after the last negative culture. There should be some clinical and microbiological follow-up to document relapse.
Thursday, July 2, 2009
Prevention of Surgical Site Infections
Today we had a case of a post-sternotomy sternal wound infection. This led to a discussion on the prevention of surgical site infections (SSI) -- nosocomial, potentially preventable infections that lead to increased morbidity and mortality, cost, and length of stay.
Keys to prevention of SSI (SHEA guidelines here):
Pre-operative mupirocin has not been shown to be beneficial for SSI (Canadian study here, larger study here) but may reduce nosocomial staph aureus infections.
No study has rigorously evaluated full pre-operative staph aureus decolonization with this protocol, which is used in Toronto for MRSA. I would probably choose to do this for elective surgeries for patients with known MRSA if there were no contraindications.
Keys to prevention of SSI (SHEA guidelines here):
- Encourage smoking cessation
- Existing infections, distant from the surgical site should ideally be treated first
- Patient should be freshly showered either before the OR or the night before, often using chlorhexadine body wash (conflicting evidence on utility, see review here)
- Hair removal, if absolutely required, should be done with clippers
- Surgical site antimicrobial prophylaxis (SSP) should be chosen based on the local epidemiology and the type of surgery
- SSP should be administered within 1 hour of the first incision, ideally before the incision. Repeat doses should be administered based on the half life of the agents involved and the length of the case. Total duration should be less than 24 hours
- Maximal attention to sterile technique and the donning of sterile gloves, gowns, masks, and hats
- Avoidance of severe (more than 11.0) hyperglycemia peri-operatively
- Avoidance of intraoperative hypothermia (less evidence)
Pre-operative mupirocin has not been shown to be beneficial for SSI (Canadian study here, larger study here) but may reduce nosocomial staph aureus infections.
No study has rigorously evaluated full pre-operative staph aureus decolonization with this protocol, which is used in Toronto for MRSA. I would probably choose to do this for elective surgeries for patients with known MRSA if there were no contraindications.
Wednesday, July 1, 2009
Infection of Cysts in Polycystic Kidney Disease
 Today we were challenged by a case of a patient with PKD who had a urinary tract infection with a resistant E. Coli complicated by a presumed infected cyst.
Today we were challenged by a case of a patient with PKD who had a urinary tract infection with a resistant E. Coli complicated by a presumed infected cyst.In PKD, renal cyst infections are usually caused by E. Coli or other urinary organisms. They can be difficult to diagnose but often present with fever, abdominal pain, and elevated inflammatory markers. Cysts may enlarge or show evidence of complex septation or debris -- however, imaging is often not helpful in making the diagnosis.
Urine culture is positive in 40%, Blood in 25%, and cyst aspirates in another 12%. Medical therapy includes a relatively prolonged (3+ weeks) course of antibiotics. Usually fluoroquinolones or TMP/SMX are preferred because of cyst penetration. Beta-lactam and aminoglycoside penetration is relatively poor.
In failure of medical therapy (prolonged symptoms, fever, sepsis) or in cases where the presumed culprit cyst is greater than 5cm in diameter, percutaneous or surgical drainage is often required.
See the recently published case series here.
In our case today we elected to use high-dose ceftriaxone (since CIP/TMP-SMZ/AMP/CEF were resistant) to try and maximize intracyst concentration.
Tuesday, June 16, 2009
Preface
I am about to embark on my first clinical rotation as a fellow in infectious diseases in Toronto. For me, this will represent the culmination of the past ten or so years of my academic and professional life.
I embark on this journey having recently spent a year as the chief resident at the Toronto General Hospital and Mount Sinai Hospital. During that time, I started a daily teaching blog based on cases taught at morning report. It was well received and served as a good informal reference. So I thought I would press my luck during my ID fellowship.
I have managed to pre-populate this blog with ID related posts from the past year and will continue on -- with daily (likely) posts on clinical topics in Infectious Diseases based upon real cases/clinical questions.
I embark on this journey having recently spent a year as the chief resident at the Toronto General Hospital and Mount Sinai Hospital. During that time, I started a daily teaching blog based on cases taught at morning report. It was well received and served as a good informal reference. So I thought I would press my luck during my ID fellowship.
I have managed to pre-populate this blog with ID related posts from the past year and will continue on -- with daily (likely) posts on clinical topics in Infectious Diseases based upon real cases/clinical questions.
Wednesday, June 10, 2009
Day # 335 - Severe Influenza
Thursday, May 28, 2009
Day #322 - Enterococcal Endocarditis
 This patient presented with stroke. This article reviews stroke in IE. This related article reviews the neurologic manifestations of IE.
This patient presented with stroke. This article reviews stroke in IE. This related article reviews the neurologic manifestations of IE.An original article by Osler on IE!
Some key points:
Mitral Valve IE ~ 10% stroke rate
Mortality is high -- 35% in hospital 52% at one year
Early antibiotic therapy reduces neurologic complications
I have previously blogged about infective endocarditis (see here) including enterococcal endocarditis. The first post goes over the Duke Criteria.
Indications for Surgical Treatment of IE (Native Valve):
- Development of heart failure
- MR/AR with dilating LV, or development of pulmonary hypertension
- Fungal IE or that caused by highly resistant organisms (think of it in MRSA)
- Patients with heart block, cardiac abscess, abnormal chamber-chamber connections
- Recurrant emboli despite ABX
- Class IIb -- large vegetations
Tuesday, May 26, 2009
Day #320 - Hypercalcemia from Presumed Sarcoid
 A great case today -- and some good topics were covered by the discussant.
A great case today -- and some good topics were covered by the discussant.1) Hypercalcemia (previously blogged here)
2) Hepatitis C and its complications including:
* Mixed cryoglobulinemia (image) which can cause a vasculitis
* Membranoproliferative glomerulonephritis (review here)
* Porphyria Cutanea Tarda
* HCV Associated Lymphoma
3) Sarcoidosis (from review)
"sarcoidosis is established on the basis of compatible clinical and radiologic findings, supported by histologic evidence [review] in one or more organs of noncaseating epithelioid-cell granulomas in the absence of organisms or particles"
"as a diagnostic tool, measurement of serum ACE levels lacks sensitivity and specificity"
Fascinating --> Evidence exists that sarcoidosis can be caused/exacerbated by HCV treatment with interferon.
Friday, May 22, 2009
Day #316 - Swine Flu
Today we heard a case of a patient with undelying Wegner's Granulomatosis who presented with several days of fever and cough. Her chest xray showed no infiltrate. The majority of patients with influenza will present with cough (90%) and fever (~70%). Headache, myalgias, arthralgias, fatigue are also common but seen in only 50-60%. There is a rational clinical exam on influenza here.
The nasopharyngeal swab revealed influenza, which was PCR confirmed to be "swine flu"
Influenza evolves by two processes. Antigenic drift, where small mutations occur over time in the surface molecules which gradualy cause waning immunity. This is the basis of seasonal influenza.
Antigenic shift invoves abrupt changes in the surface molecules, often as a conseuqnce of recombination with swine or avian lineages, into a strain to which few in the population are likely to have immunity. This leads to epidemic (and pandemic) influenza.

Treatment of Influenza:
- Supportive care
- In patients admitted to hospital/ICU or those with severe disease or severe undelying co-morbidities should receive antiviral therapy (also give to healthy people with less than 72h of symptoms)
- Oseltamavir (neuraminadase inhibitor -- blocks entry of virus into cell) --> available orally, circulating H1N1 are resistant, circulating H3N2 are likely resistant.
- Zanamavir (neuraminadase inhibitor) --> inhalational only, all are currently succeptible
- Amandadine (M channel inhibitor) --> blocks release of viral RNA into the cytoplasm from the lysosome. Available orally, most H3N2 resistant, many H1N1 succeptible.
Thursday, May 21, 2009
Day #315 - Sepsis with DIC
 Today we discussed a great case of SEPSIS (focus of infection unclear) with associated DIC.
Today we discussed a great case of SEPSIS (focus of infection unclear) with associated DIC.SIRS Criteria:
Fever or hypothermia
WBC >12,000 or less than 4,000
HR >90
RR >20
Sepsis = 2 or more SIRS criteria of presumed infective etiology
Severe sepsis includes sepsis with end organ dysfunction or lactate >4
Septic shock includes severe sepsis with refractory hypotension requiring inopressors
I have blogged about Early Goal Directed therapy here. Source control is as essential as broad spectrum antibiotics in the treatment of sepsis.
These are recent guidelines on the diagnosis and management of DIC here. Transfusion of plateletes and factors is limited to patients who are bleeding or at high risk of bleeding (i.e. post-op), therapeutic heparins are limited to patients who have thrombosis, DVT prophylaxis is required.
Wednesday, May 20, 2009
Day #314 - Pulmonary Eosinophilia
 Very complex case facilitated by an expert discussant. The key focus, other than on the case at hand was a demonstration of clinical reasoning and Bayes theorem.
Very complex case facilitated by an expert discussant. The key focus, other than on the case at hand was a demonstration of clinical reasoning and Bayes theorem. We highlighted the importance of Occam's Razor -- but stressed the importance of recognizing Hickam's dictum.
I have previously blogged about pulmonary eosinophilia here (with references). In my mind, an important consideration in this patient (given travel to China) is to exclude disseminated strongyloidiasis because like infliximab related interstitial lung disease (NEJM article here) 'strongy' can appear to improve on steroids.
This is a recent review from the Lancet on TNF-alpha blockade and the interaction with tuberculosis.
NB: Review of radiographic manifestations of pulmonary TB.
Tuesday, May 12, 2009
Day #306 - TB Pleuritis

We discussed a great case of tuberculosis causing pleural effusion today. I have previously blogged about this before.
Previous blogs on pleural effusion here and here (including discussion of Light's Criteria and parapneumonic effusions/empyema).
Modified Light's Criteria (see review here):
- Change LDH pleural fluid 0.45 ULN (increases sensitivity but reduces specificity)
Alternative tests:
- LDH (0.45ULN), cholesterol (45mg/dl) and protein (29g/L) of pleural fluid, done in combination have similar performance characteristics to Light's criteria and don't require paired serum samples.
Monday, May 11, 2009
Day #305 - HIV Lymphoma
Today we discussed a case of a patient with known HIV disease (CD4 300-500, not on therapy) who presented with fever, diffuse adenopathy, and splenomegaly. The presumed cause is lymphoma.
The differential diagnosis would include:
Infections:
- HIV with high level viremia
- Mononucleosis syndromes (EBV, CMV, acute toxoplasmosis)
- Syphilis
- Disseminated TB
- In the more immunosuppressed host:
- Mycobacterium Avium Complex
- Bartonella Henselae
- Disseminated fungal infection (i.e. histoplasmosis)
- Non-infectious
- Lymphoma
- Multicentric Castleman's Disease
- Sarcoidosis
- Lymphoma
I have previously blogged about HIV here, here (with cryptococcal meningitis), and here (with PCP pneumonia).
I have blogged about lymphoma including staging here.
A review of the pathology of HIV associate lymphomas is here. An article reviewing the treatment of HIV associated lymphoma is here.
Tuesday, May 5, 2009
Day #299 - Enterococcal Prosthetic Valve Endocarditis

Great case. I have previously blogged about the diagnosis of endocarditis here and here.
Patient with multiple prosthetic valves develops sepsis in the context of an enterococcal bacteremia. Highly suspicious though non diagnostic echo for PVIE. Treated with VANCOMYCIN ("penicillin allergy" is a pet peeve of mine) and GENTAMICIN (for synergy). The evidence for synergy is not totally supported by clinical experience. Nephrotoxiciy is common but similarly has not been shown to impact mortality. The combination of VANCOMYCIN with an aminoglycoide increases the risk of nephrotoxicity.
We also reviewed aminoglycoside ototoxicity -- presenting either as sensory-neuro hearing loss or vestibulary dysfunction.
This patient developed renal failure presumably related to ATN from the VANCO+GENT; however, one can get a glomerulonephritis in endocarditis.
There is evidence that AMPICILLIN plus CEFTRIAXONE (which usually has no enterococcal coverage) can be used effectively in the treatment of enterococcal endocarditis.
Patient with multiple prosthetic valves develops sepsis in the context of an enterococcal bacteremia. Highly suspicious though non diagnostic echo for PVIE. Treated with VANCOMYCIN ("penicillin allergy" is a pet peeve of mine) and GENTAMICIN (for synergy). The evidence for synergy is not totally supported by clinical experience. Nephrotoxiciy is common but similarly has not been shown to impact mortality. The combination of VANCOMYCIN with an aminoglycoide increases the risk of nephrotoxicity.
We also reviewed aminoglycoside ototoxicity -- presenting either as sensory-neuro hearing loss or vestibulary dysfunction.
This patient developed renal failure presumably related to ATN from the VANCO+GENT; however, one can get a glomerulonephritis in endocarditis.
There is evidence that AMPICILLIN plus CEFTRIAXONE (which usually has no enterococcal coverage) can be used effectively in the treatment of enterococcal endocarditis.
Friday, May 1, 2009
Day #295 - Tuberculosis and Immune Reconstitiution

We discussed a case of pulmonary and extrapulmonary tuberculosis which presented on TNF-alpha antagonist therapy.
Addendum: TB Immune Reconstitution Reviewed Recently here.
We also discussed paradoxical worsening of TB post-discontinuation of immunosuppression. The case report I was talking about is available here.
Subscribe to:
Posts (Atom)




