(I'm not providing you with medical advice. Clinical correlation and professional interpretation required)
Tuesday, November 9, 2010
If you don't take the temperature, the patient can't have a fever...
This article reminded me of one of the fatman's rules from Shem's novel. In this study, computer rule generated central line infection rates were significantly higher than those reported by infection control teams -- in the modern era of reporting and pay for performance, one does wonder if, given a case that is grey one may be more inclined to call it black or white.
Tuesday, October 5, 2010
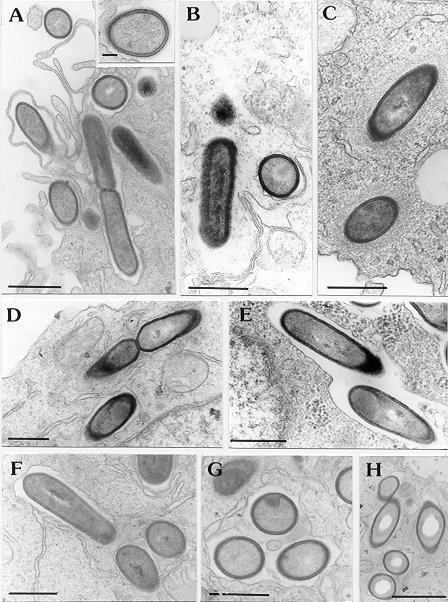
Blastomycosis
I saw a case of cutaneous blastomycosis in clinic today -- two lesions, one on the face, the other on the buttock in an otherwise healthy male patient. A nice review is here.
Blastomycosis is a dimorphic (mould at room temperature, yeast at body temperature) fungus which is endemic in certain geographic areas of North America. Ontario, where I currently live, and in particular northwest Ontario by the Manitoba border is one such geographic hot spot.
The most common sites of infection are:
Blastomycosis is a dimorphic (mould at room temperature, yeast at body temperature) fungus which is endemic in certain geographic areas of North America. Ontario, where I currently live, and in particular northwest Ontario by the Manitoba border is one such geographic hot spot.
The most common sites of infection are:
- Pulmonary (most patients have some pulmonary involvement)
- Presents as acute (including ARDS) or chronic pneumonia, pulmonary nodule, asymptomatic
- Cutaneous (in 40-80% of cases) presenting as verrucous or ulcerative skin lesions (like my patient)
- Osteomyelitis (~25% of extrapulmonary) presenting as painful lesion in bone, which can mimic sarcoma in radiographic appearance. Occasionally can have concomittant septic arthritis in adjacent bone.
- GU: (10-30%) in men prostate, testicle, epididymis.
- CNS (5-10%), usually chronic meningitis, occasionally space occupying lesions
- Other
Saturday, July 24, 2010
New HIV Guidelines
vailable July 21 issue of JAMA (free, please read the full article from there).
Not sure I agree with all recommendations. This is the curse of 'growing up' in medicine and therefore developing your own opinion.
I think it is too early to consider raltegravir (and maybe even darunavir) as first line therapies in treatment naive patients. Especially with other options available. The authors hint at this point but are not explicit enough for the audience of the guideline (in my humble opinion)
Likewise for starting with CD4 greater than 500. Those patients should be enrolled in properly designed prospective studies (hence the CIII recommendation)
Not sure I agree with all recommendations. This is the curse of 'growing up' in medicine and therefore developing your own opinion.
I think it is too early to consider raltegravir (and maybe even darunavir) as first line therapies in treatment naive patients. Especially with other options available. The authors hint at this point but are not explicit enough for the audience of the guideline (in my humble opinion)
Likewise for starting with CD4 greater than 500. Those patients should be enrolled in properly designed prospective studies (hence the CIII recommendation)
Monday, July 5, 2010
Format revision and Candidemia Line Removal
Since I have left the clinical ID teaching service as a fellow -- hopefully to return as faculty in 2011, I will slightly alter the blog format. I will highlight interesting cases that I see in my individual practice, and will highlight what I think are interesting/notable articles in the current literature.
This week's post:
Challenging dogma: Central lines may not need to be removed early in candidemia???
Subgroup analysis of 2 RCTs in treatment of candidemia (mainly echinocandin and lipid ampho B used)
Looked at removal 24-48h vs. later removal vs. retention
842 total, 354 removed early 180 removed late 304 retained
Note that it appears in multivariate analysis that CVC removal was not associated with treatment success or mortality. But the point estimates are in favor of removal and the CI's are wide.
In the univariate analysis CVC removal within 48h was associated with improved survival.
Why? Were sicker patients having their lines retained leading to the perception of increased mortality (that was adjusted for in the multivariate analysis). Statistical confounding?
The associated editorial is worth reading.
I also see candidemia reported -- but not other metastatic complications such as endopthamitis, which would be clinically relevant but not noted in surveilance blood cultures.
Bottom line: An interesting read that challenges dogma, and I think lends itself to further analysis with large enough numbers and robust enough data to exclude a meaningful clinical benefit of earlier removal.
Until then -- please remove my line promptly should I ever have a CVC related candidemia.
This week's post:
Challenging dogma: Central lines may not need to be removed early in candidemia???
Subgroup analysis of 2 RCTs in treatment of candidemia (mainly echinocandin and lipid ampho B used)
Looked at removal 24-48h vs. later removal vs. retention
842 total, 354 removed early 180 removed late 304 retained
Note that it appears in multivariate analysis that CVC removal was not associated with treatment success or mortality. But the point estimates are in favor of removal and the CI's are wide.
In the univariate analysis CVC removal within 48h was associated with improved survival.
Why? Were sicker patients having their lines retained leading to the perception of increased mortality (that was adjusted for in the multivariate analysis). Statistical confounding?
The associated editorial is worth reading.
I also see candidemia reported -- but not other metastatic complications such as endopthamitis, which would be clinically relevant but not noted in surveilance blood cultures.
Bottom line: An interesting read that challenges dogma, and I think lends itself to further analysis with large enough numbers and robust enough data to exclude a meaningful clinical benefit of earlier removal.
Until then -- please remove my line promptly should I ever have a CVC related candidemia.
Tuesday, April 20, 2010
We spoke today about Group A Streptococcus (Streptococcus pyogenes). I thought it would be reasonable to quickly review rheumatic fever (see review).
Diagnosis (Jones Criteria):
MAJOR:
Carditis
Arthralgia
Fever
Elevated CRP
Prolonged PR interval
Diagnosis: 2 major or 1 major 2 minor. Debate as to how sensitive these criteria are -- and they may lead to undertreatment/diagnosis.
Note: At time of diagnosis up to 75% will be culture negative. Usually happens about 2-3 weeks post infection. The ASOT can be helpful (but isn't perfect and many labs don't do it anymore) particularly if it rises with 2 samples taken 2 weeks apart.
See previous blog about peripartum sepsis and toxic shock syndrome including treatment thereof.
See necrotizing fasciitis described in this blog including role of IVIG and prophylaxis of close contacts.
Diagnosis (Jones Criteria):
MAJOR:
Carditis
- Can affect pericardium, myocardium, endocardium, and epicardium. Pericardium: pleuritic chest pain, pericarditis. Endocardium: usually new mitral regurgitation. Epicardium: Conduction abnormalities. Myocardium: Can mimic myocarditis.
- Knees, elbows, ankles, wrists. Often overlapping and migratory.
- Often unilateral chorea. Emotional lability. Weakness. Sensory change is not seen.
- Evanescent, pink rash with circumsribed borders. Usually on trunk/arms.
- Painless with normal overlying skin on bony surfaces and tendon. A few mm to 1cm in size. Usually 3-4 and symmetric.
Arthralgia
Fever
Elevated CRP
Prolonged PR interval
Diagnosis: 2 major or 1 major 2 minor. Debate as to how sensitive these criteria are -- and they may lead to undertreatment/diagnosis.
Note: At time of diagnosis up to 75% will be culture negative. Usually happens about 2-3 weeks post infection. The ASOT can be helpful (but isn't perfect and many labs don't do it anymore) particularly if it rises with 2 samples taken 2 weeks apart.
See previous blog about peripartum sepsis and toxic shock syndrome including treatment thereof.
See necrotizing fasciitis described in this blog including role of IVIG and prophylaxis of close contacts.
Friday, April 16, 2010
Penicillin Allergy

Not to be understated in terms of potential severity, it is true that the number of penicillin 'allergic' patients far outnumbers the number of patients with an actual allergy to penicillin.
The validity of allergies to penicillin recorded in the chart is questionable. The JAMA classic article on history of pencillin allergy is here.
This study (and others) shows meropenem is *likely* safe in patients with IgE mediated penicillin allergy.
The following review article discusses the use of other agents and a strategy for evaluating patients with penicillin allergy. This review discusses antibiotic allergies in general.
***
The ACLS guidelines for the management of anaphalaxis are here.
Delusional Parasitosis
Interesting case today -- and sad. Delusional parasitosis can be very difficult to treat and can be debilitating for patients. There is a role for consult liason psychiatry and newer generation antipsychotics (see review here).
An interesting case report of IATROGENIC delusional parasitosis (i.e. patient believed she had infestation because her doctors told her she did) is here.
An interesting case report of IATROGENIC delusional parasitosis (i.e. patient believed she had infestation because her doctors told her she did) is here.
Surgery for Infective Endocarditis

Recent publication in circulation addresses the issue very well.
For the cutting edge -- vegetectomy (removal of vegetation) without valve replacement may be an option worthy of study.
See previous posts on IE for more info on IE.
Thursday, April 15, 2010
PCP with steroids
Frequently invoked, rarely proven the development of PCP with steroid therapy is rare but important to consider.
TMP/SMX prophylaxis for PCP in patients on high dose steroids (Table below) from this meta-analysis. In general, though there is no consensus, PCP prophylaxis should be considered in patients on greater than 30mg of prednisone for greater than three months or those who are on moderate-high dose steroids with another immunosuppressive agent (i.e. patients with Wegner's)

However, the story may be different in lymphoma treatment, particularly with rituximab and high dose CHOP therapy but overall is also low in hematologic (exclude ALL) and solid organ malignancy.
TMP/SMX prophylaxis for PCP in patients on high dose steroids (Table below) from this meta-analysis. In general, though there is no consensus, PCP prophylaxis should be considered in patients on greater than 30mg of prednisone for greater than three months or those who are on moderate-high dose steroids with another immunosuppressive agent (i.e. patients with Wegner's)

However, the story may be different in lymphoma treatment, particularly with rituximab and high dose CHOP therapy but overall is also low in hematologic (exclude ALL) and solid organ malignancy.
Vancomycin Nephrotoxicity
 A review of vancomycin nephrotoxicity is available here.
A review of vancomycin nephrotoxicity is available here.The IDSA guidelines for therapeutic drug monitoring of vancomycin here.
The first vancomycin trough achieved seems to have predictive value for who will develop nephrotoxicity.
The role of dialysis in acute vancomycin mediated renal injury is discussed here (little evidence from which to draw conclusions, but seems reasonable).
Tuesday, March 16, 2010
Recurrent HSV Encephalitis
Interesting case. Second episode of Herpes Simplex encephalitis in an adult approximately 3 years after the first. Here is a case report and literature review on recurrent disease.
The main deteminant of outcome in HSV encephalitis is time to acyclovir. This article discusses factors associated with the delay of administration.
This article discusses the outcomes of HSV in population based study.
I discuss viral encephalitis in a previous blog.
The main deteminant of outcome in HSV encephalitis is time to acyclovir. This article discusses factors associated with the delay of administration.
This article discusses the outcomes of HSV in population based study.
I discuss viral encephalitis in a previous blog.
Tuesday, March 9, 2010
Neutropenic Entercolysis
With thanks for the suggestion.
Today we saw a patient with lymphoma, status post bone marrow transplant, who developed fever, neutropenia, abdominal pain, diarrhea and colitis on CT scan with a presumed diagnosis of neutropenic enterocolitis.
This condition, loosely defined (but best defined as fever, abdominal pain and colonic thickening -- see here) is seen in about 5% of patients. The mortality approaches 50% in some studies.
Ultrasound may be useful in screening for this condition early on.
Usual pathogens are bacterial (gram negative bowel flora including pseudomonas, and gram positive bowel flora). Bacteremia is seen in 35-80% of cases. A reasonable coverage choice would be an anti-pseudomonal beta-lactam (i.e. piperacillin-tazobactam or meropenem) with anerobic activity, or something like ceftazadime with metronidazole.
Fungal infection is rare (~5%) and usually candidal, but caries a high mortality (~80% in some studies). Emperic antifungal coverage should be considered if still febrile and neutropenic at 5 days or in the severely ill.
Critically ill patients should be considered for colectomy as should patients with complications (megacolon, perforation).
Today we saw a patient with lymphoma, status post bone marrow transplant, who developed fever, neutropenia, abdominal pain, diarrhea and colitis on CT scan with a presumed diagnosis of neutropenic enterocolitis.
This condition, loosely defined (but best defined as fever, abdominal pain and colonic thickening -- see here) is seen in about 5% of patients. The mortality approaches 50% in some studies.
Ultrasound may be useful in screening for this condition early on.
Usual pathogens are bacterial (gram negative bowel flora including pseudomonas, and gram positive bowel flora). Bacteremia is seen in 35-80% of cases. A reasonable coverage choice would be an anti-pseudomonal beta-lactam (i.e. piperacillin-tazobactam or meropenem) with anerobic activity, or something like ceftazadime with metronidazole.
Fungal infection is rare (~5%) and usually candidal, but caries a high mortality (~80% in some studies). Emperic antifungal coverage should be considered if still febrile and neutropenic at 5 days or in the severely ill.
Critically ill patients should be considered for colectomy as should patients with complications (megacolon, perforation).
Thursday, February 25, 2010
Enterococcal Endocarditis
We saw a case of aortic and mitral valve enterococcal endocarditis.
Previous endocarditis blogs here with associated links.
While not really studied, there are some limited case reports or in vitro data for the possibility of:
Though any of the above agents should primarily be used in the context of clinical trial or 'dire cicrumstances'
Previous endocarditis blogs here with associated links.
While not really studied, there are some limited case reports or in vitro data for the possibility of:
- Daptomycin (also retrospective review in bacteremia here)
- Linezolid (and in general review of linezolid in IE here)
- Ceftobiprole (NB it lost its FDA approval in April 2010!)
Though any of the above agents should primarily be used in the context of clinical trial or 'dire cicrumstances'
Tuesday, February 16, 2010
Friday, February 5, 2010
Epidural Abscess
 We have seen a number of cases of epidural abscess this week. Reviews here (Lancet Neurology), and here (NEJM). Not to be confused with the coolest name in medicine Pott's puffy tumour as described here.
We have seen a number of cases of epidural abscess this week. Reviews here (Lancet Neurology), and here (NEJM). Not to be confused with the coolest name in medicine Pott's puffy tumour as described here.Epidemiology:
- Rare - about 0.2 to 2 per 10,000 admissions
- Often underlying condition:
- Diabetes
- Alcoholism, Injection Drug Use
- HIV
- Chronic spine disease
- Previous spine surgery
- Indwelling catheters
- Contiguous spread of infection from soft tissue/vertebrae/manipultion (~30%)
- Hematogenous seeding ~50%
- Unknown 15%
- Can injure spinal cord leading to paralysis due to compression (local) or small septic emboli causing infarction.
- Most ~60% are Staphylococcus aureus including MRSA
- Can be CNST if hardware in situ
- E. coli from bacteremic urinary tract infection
- Pseudomonas (often injection drug use)
- Other: enterococcus, viridans group streptococcus, mycobacteria, fungus (candida, other) etc.
History:
- Pain is common, initially localized, then radicular and referred (85%)
- Increasing weakness as cord is involved and sensory loss
- Bladder and bowel involvement occur later then fullparalysis
- Fever may be absent! Especially if NSAIDS or acetominophen for pain
- Normal WBC in up to 40%!
- Most have elevated CRP and ESR
- Bacteremia in up to 60%
- MRI is test of choice.
- Concomittant osteomyelitis seen in ~80%. This may be seen on CT; but the abscess can be missed with plain CT.
- If stable and no imminent neurologic comprimise, it is best to get a definitive diagnosis. Blood cultures should be sent and operative specimens. Then antibiotics can be started tailored to the etiologic agent.
- Usually combined medical and surgical management is required. The deficits can progress exceptionally quickly (i.e. complete paralysis within hours) and can be irreversible (particularly if paralysis has been for more than 36 hours!
- If empiric coverage is required, coverage for Staphylococcus aureus, including MRSA as well as gram negatives should be started. Antipseudomonal coverage may be required if there is a risk for pseudomonas -- i.e. IDU, known pseudomonas elsewhere.
- One reasonable approach would be to start VANCOMYCIN (MRSA) and either CEFEPIME, PIPERACILLIN-TAZOBACTAM, or CEFTAZADIME

Prognosis:
- Paralysis will develop in 4-22%. Paralysis is likely to be irreversible after 24-36 hours
- With prompt surgery most patients have as good or better neurologic status than they did before the OR.
- Death does occur in about 5%
Tuesday, February 2, 2010
MRSA pneumonia
 Today we saw a case of severe methicillin resistant staphylococcus aureus (MRSA) pneumonia (review). In the era of community acquired (CA-MRSA), this is becoming a significant problem.
Today we saw a case of severe methicillin resistant staphylococcus aureus (MRSA) pneumonia (review). In the era of community acquired (CA-MRSA), this is becoming a significant problem.Management includes:
- Supportive care in keeping with best practices
- Vancomycin is the 'gold standard' -- but not a great one.
- aim for trough ~ 20
- avoid in MIC greater than or equal to 2 (and maybe even 1)
- addition of rifampin improves short term microbiologic cure, but interestingly was associated with increased long term mortality
- Alternatives include:
- Linezolid -- often postulated, not yet proven to be superior.
- the maker of linezolid was fined for off label marketing of the drug for the use in MRSA pneumonia (see one example news article here) so caveat emptor...
- Tigecycline -- theorhetically 'better' lung kinetics than vancomycin -- not studied
- Ceftobiprole -- under study. Has advantages in terms of tissue penetration and the fact that it is a beta-lactam
- doxycycline or TMP/SMX -- could be an option for milder disease.
- Daptomycin -- do not use, inferior.
- Linezolid -- often postulated, not yet proven to be superior.
- Duration of therapy 8-14 days (or longer in bacteremia with other focus) depending on resolution of clinical symptoms. Some studies show no difference between 8 and 15 days of therapy. Many experts 'prefer' 14 days.
Monday, February 1, 2010
Necrotizing Fasciitis
 Today we saw a case of necrotizing fasciitis (see previously blogged). This case was in the abdominal wall and perineum of a female patient with obesity and diabetes, and is likely polymicrobial (type I).
Today we saw a case of necrotizing fasciitis (see previously blogged). This case was in the abdominal wall and perineum of a female patient with obesity and diabetes, and is likely polymicrobial (type I).While people often use 'Fournier's' gangrene to infer disease in males that involves the scrotum, the disease entity, involving the pereneum does occur in women. In fact, women seem to have higher mortality, possibly because of involvement of the retroperitoneal space due to anatomic differences and also due to delays in diagnosis. This article also suggests that disease in females is underrecognized, and that ano-rectal disease is far more dangerous precipitant than urological disease.
Death and amputation are more likely at extremes of age, with advancing comorbidities (including diabetes), with sepsis, and with visible gangrene on presentation.
Wednesday, January 27, 2010
CMV Esophagitis
Today we saw a case of a patient with renal transplant who developed CMV esophagitis and also has a newly diagnosed high grade B-cell neoplasm in need of chemotherapy.
This raised a number of questions which I have attempted to answer with the associated references.
1) How do we manage this patient?
2) When can we safely provide cancer treatment?
3) Why did this happen?
The American Journal of Transplantation has a set of guidelines which has recently been updated. The guidelines for CMV prevention and treatment are available here. These guidelines are similar, but in the bone marrow transplant population.
This article looks at risk factors in renal transplantation for developing CMV disease.
This article addresses what happens to patients with pre-existing CMV disease (or recently treated) who go on to SCTx.
Finally, this article describes/summarizes post transplant lymphoproliferative disorder (PTLD) which this patient's lymphoma likely is related to.
This raised a number of questions which I have attempted to answer with the associated references.
1) How do we manage this patient?
2) When can we safely provide cancer treatment?
3) Why did this happen?
The American Journal of Transplantation has a set of guidelines which has recently been updated. The guidelines for CMV prevention and treatment are available here. These guidelines are similar, but in the bone marrow transplant population.
This article looks at risk factors in renal transplantation for developing CMV disease.
This article addresses what happens to patients with pre-existing CMV disease (or recently treated) who go on to SCTx.
Finally, this article describes/summarizes post transplant lymphoproliferative disorder (PTLD) which this patient's lymphoma likely is related to.
Tuesday, January 26, 2010
Choramnionitis with Beta-Hemolytic Strep Bacteremia
Today we discussed a case of presumed choramnionitis with beta-hemolytic strep bacteremia. I have previously blogged about GBS here and peripartum GAS infection here.
This article, while basic, is a reasonable review of the role on parenteral antibiotics in peripartum women with fever. I would probably choose slightly different antibiotics if giving more than one/two doses. This article discusses the differential diagnosis of peripartum fever.
This cochrane meta-analysis questions the practice of peripartum prophylaxis in known GBS patients... I'm still convinced it is a good idea.
This article, while basic, is a reasonable review of the role on parenteral antibiotics in peripartum women with fever. I would probably choose slightly different antibiotics if giving more than one/two doses. This article discusses the differential diagnosis of peripartum fever.
This cochrane meta-analysis questions the practice of peripartum prophylaxis in known GBS patients... I'm still convinced it is a good idea.
Monday, January 25, 2010
Varicella Pneumonia
 Today we saw a case of disseminated varicella with associated varicella pneumonia / pneumonitis. This was in the context of a primary infection in an adult patient.
Today we saw a case of disseminated varicella with associated varicella pneumonia / pneumonitis. This was in the context of a primary infection in an adult patient.This is a review of varicella pneumonitis, and a link to an article discussing the contraversial role of corticosteroids in its treatment.
Varicella can also cause a number of end organ specific syndromes including:
- myopericarditis
- retinitis
- meningitis and meningoencephalitis.
- transverse myelitis
- pancreatitis
- hepatitis
- Ramsey Hunt Syndrome (? role for treatment with antivirals)
- Role for caution with steroids in the absence of antivirals for proven RHS?
- Role for caution with steroids in the absence of antivirals for proven RHS?
There are guidelines of management and a good review of various syndromes published here.
Previous related blogs are here and here.
Thursday, January 21, 2010
Clostridium difficile smorgasboard

See previous blogs here.
And now for a smattering of interesting C. difficile associated publications since the last time I posted on this topic...
- An entire issue of the journal Anaerobe dedicated to C. difficile related issues is available here.
Notable articles in this journal include:- reviews of diagnostic testing
- probiotics (lack of efficacy in prevention and treatment according to the authors)
- fecal transplant (suggests that it does indeed work -- even if gross)
- the 'rixamixin chaser' (shows promise in multiple relapses, but not the magic bullet
- The potential role of an antitoxin (NEJM here)
- The development of disease in patients status post collectomy!
- The perils and difficulties of diagnosis.
- EIA sensitivity is relatively poor - ~60-70%
- GDH has better sensitivity, but poor specificity
- Cytotoxic assays are time consuming and expensive
- PCR may be less effort dependent but has an upfront cost
- An algorithm suggested is GDH as a screen, if positive confirm with EIA, if negative EIA do PCR or cytotoxic assay.
- A set of european guidelines, which seem quite reasonable.
- An article on the challenges of treating patients in the ICU including:
- lack of sensitivity of testing means potential undertreating of critically ill patients
- the role of vancomycin in severe disease
- the absence of diarrhea (as also reported from Toronto) in up to 20% of critically ill patients because of illeus, post-operative status, or narcotics
Wednesday, January 20, 2010
Candida Endopthalmitis
We've talked about candidemia before...
One of the complications of candidemia is the development of endogenous endopthalmitis. Different rates of occular involvement are quoted from 2%-40% depending on case series.
The majority of patients will develop endopthamitis within 2 weeks of candidemia. Particularly if there is a delay in treatment of the candidemia or if the candidemia is protracted.
One of the complications of candidemia is the development of endogenous endopthalmitis. Different rates of occular involvement are quoted from 2%-40% depending on case series.
The majority of patients will develop endopthamitis within 2 weeks of candidemia. Particularly if there is a delay in treatment of the candidemia or if the candidemia is protracted.
Early retinal exam can diagnosis, but follow up at 2 weeks is prudent as early lesions can be missed.
Treatment is covered in the IDSA guidelines (previously cited). Azole agents can be used for succeptible isolates. If there is a significant vitritis, sometimes vitrectomy with intraoccular amphotericin is required in addition to systemic therapy.
There are a number of good reviews here (treatment), here (case report and review of condition), here (BMJ review) and here (retinal lesions in sepsis, including description of occular manifestations).
Treatment is covered in the IDSA guidelines (previously cited). Azole agents can be used for succeptible isolates. If there is a significant vitritis, sometimes vitrectomy with intraoccular amphotericin is required in addition to systemic therapy.
There are a number of good reviews here (treatment), here (case report and review of condition), here (BMJ review) and here (retinal lesions in sepsis, including description of occular manifestations).
Tuesday, January 19, 2010
Klebsiella pneumoniae carbepenemase
We've talked a lot about this one -- but fortunately have yet to see one.
Some useful reviews/information:
Some useful reviews/information:
Monday, January 18, 2010
Cryoglobulinemia related to HCV
This weekend we saw a case of presumed cryoglobulemic vasculitis in a patient with known HCV. There is a previous blog related to HCV here, including a good link to a review on cryoglobulinemia. The following figure on causes of cryoglobulenemia is taken from said review:

Another review, particularly related to HCV is available here. In patients with HCV associated cryoglobulinemia, treatment of the HCV may be helpful in getting the condition under control.

Another review, particularly related to HCV is available here. In patients with HCV associated cryoglobulinemia, treatment of the HCV may be helpful in getting the condition under control.
Friday, January 15, 2010
Thursday, January 14, 2010
Histoplasmosis (actually was sporothrix!)
 Fascinating case today -- patient who works in construction who presented to hospital initially with hilar adenopathy, erythema nodosum and ankle arthritis who was initially diagnosed with sarcoidosis, but who went on to develop disseminated histoplasmosis with steroid therapy.
Fascinating case today -- patient who works in construction who presented to hospital initially with hilar adenopathy, erythema nodosum and ankle arthritis who was initially diagnosed with sarcoidosis, but who went on to develop disseminated histoplasmosis with steroid therapy.Histoplasmosis mimicing sarcoidosis with EN and arthritis has been described here and has been dubbed 'pseudosarcoidosis'. It has also been described here and here.
Several good reviews of histoplasmosis are available (here, and here- mainly pulmonary).
Manifestations include (but are not limited to):
- Asymptomatic -- majority!
- Acute pulmonary histoplasmosis
- Usually self-limited febrile illness with respiratory symptoms. Mediastinal lymphadenopathy common. Can have erythema nodosum and be mistaken for sarcoidosis.
- Mild forms do not require treatment.
- Chronic cavitary pulmonary histoplasmosis
- Granulomatous mediastinitis
- large necrotic mediastinal nodes cause compressive symptoms
- large necrotic mediastinal nodes cause compressive symptoms
- Fibrosing mediastinitis
- Pericarditis
- Disseminated (Systemic) Disease
- Ususally immunosuppressed patients: AIDS (CD4 below 150), hematologic malignancies, transplant patients, steroids, TNF alpha inhibitors, congenital immunodeficiencies
- May occur during initial infection or as reactivation event years later
- Every organ system may be involved. Commonly, fever, arthralgias, anorexia, malaise. Pancytopenia, hepatosplenomegaly. GI involvement with diarrhea common.
- Endocardtitis/endovascular
- CNS disease
Addendum:
- Even more interesting -- the case turns out to be sporothrix schenckii instead of histoplasma!
- See description of sporothrix mimicking sarcoid here, and IDSA guidelines for sporothrix here. There are no published cases like ours to date -- expect that to change.
- According to this article -- Amphotericin B and itraconazole are the most active. Voriconazole is not active, nor is fluconazole.
Wednesday, January 13, 2010
Bilateral leg 'cellulitis'
A number of consults for this clinical entity today makes me want to provide you with this excelllent review of the mimickers of cellulitils.... The most common mimicker I see is venous stasis dermatitis, often bilateral, in the obese patient with heart failure.
Tuesday, January 12, 2010
Peripartum sepsis with Group A Streptococcus
Today we saw a case of group A streptococcal bacteremia associated with peripartum sepsis and intrabdominal abscesses. This is similar to a case reviewed here (and here). NEJM case report here.
The case definition (epidemiologic) for streptococcal toxic shock syndrome (CDC) includes:
Treatment includes supportive care, debridement of necrotic/non-viable tissues and source control , consideration of IVIG , and antibiotic therapy with beta-lactam (i.e. penicillin) with clindamycin (for its anti-ribosomal activity and effect on non-log phase growth); however, recent data suggests that exotoxin production may actually be increased if the organism is clindamycin resistant. Linezolid may be an alternative anti-ribosomal agent in this case.
The case definition (epidemiologic) for streptococcal toxic shock syndrome (CDC) includes:
- hypotension defined by a systolic blood pressure less than or equal to 90 mm Hg for adults
- Multi-organ involvement characterized by two or more of the following:
- Renal impairment: Creatinine greater than or equal to 2 mg/dL (greater than or equal to 177 µmol/L) for adults. In patients with preexisting renal disease, a greater than twofold elevation over the baseline level.
- Coagulopathy: Platelets less than or equal to 100,000/mm3 (less than or equal to 100 x 106/L) or disseminated intravascular coagulation, defined by prolonged clotting times, low fibrinogen level, and the presence of fibrin degradation products.
- Liver involvement: Alanine aminotransferase, aspartate aminotransferase, or total bilirubin levels greater than or equal to twice the upper limit of normal for the patient's age. In patients with preexisting liver disease, a greater than twofold increase over the baseline level.
- Acute respiratory distress syndrome: defined by acute onset of diffuse pulmonary infiltrates and hypoxemia in the absence of cardiac failure or by evidence of diffuse capillary leak manifested by acute onset of generalized edema, or pleural or peritoneal effusions with hypoalbuminemia.
- A generalized erythematous macular rash that may desquamate.
- Soft-tissue necrosis, including necrotizing fasciitis or myositis, or gangrene.
Treatment includes supportive care, debridement of necrotic/non-viable tissues and source control , consideration of IVIG , and antibiotic therapy with beta-lactam (i.e. penicillin) with clindamycin (for its anti-ribosomal activity and effect on non-log phase growth); however, recent data suggests that exotoxin production may actually be increased if the organism is clindamycin resistant. Linezolid may be an alternative anti-ribosomal agent in this case.
Friday, January 8, 2010
Candidemia redux
See previous blog. Today we saw a patient with candidemia, presumably from a urinary source. We discussed species identification, and the use of the germ tube test for rapid identification of Candida albicans.
This article discusses the clinical utility of the germ tube test, quoting a sensitivity of 87% and specificity of 100% for identifing C. albicans -- directly off of the positive blood culture! This saves ~24h in the rapid identification of C. albicans, as the germ tube is traditionally performed off a subculture on fungal medium, adding up to a 24h delay.
This article discusses the clinical utility of the germ tube test, quoting a sensitivity of 87% and specificity of 100% for identifing C. albicans -- directly off of the positive blood culture! This saves ~24h in the rapid identification of C. albicans, as the germ tube is traditionally performed off a subculture on fungal medium, adding up to a 24h delay.
Thursday, January 7, 2010
Strongyloides
 Previously mentioned 'strongy' here. CMAJ reviews here, and here.
Previously mentioned 'strongy' here. CMAJ reviews here, and here.There was an extensive discussion at case-rounds yesterday afternoon about prophylaxis for strongyloidiasis in patients at risk who will be immunosuppressed.
Here is a review of strongyloidiasis in the immunocomprimised patient.
This article discusses prevention in patients with connective tissue diseases.
In patients with bone marrow transplantation or solid organ transplantation recent guidelines suggest that patients with unexplained eosinophilia or who have lived/travelled in areas endemic for strongyloidiasis, even if remotely, should be screened prior to transplant with stool O&P time three and serology. Positive screening or eosinophilia should prompt pre-emptive treatment prior to transplant with ivermectin. Mind you, some experts would suggest, given the few side effects, that people who have lived in endemic areas should just be treated...
Recent case report of death due to strongyloides in patient with HSCT...
Wednesday, January 6, 2010
TB - Tuberculosis Hodge-podge
Yesterday we saw an interesting case at the end of the day of a patient on immunosuppression who presented with a new left sided pleural effusion and some parenchymal changes compatible with a flare of her underlying lung disease vs. tuberculosis.
This patient comes from an endemic country and has evidence of fibronodular changes on chest x-ray (RR for reactivation ~15). There has been no previous TB treatment.
This highlights a large number of good teaching points:
- Diagnosis and management of latent TB.
- Diagnostic approach to possible TB pleuritis.
- The interplay between TB and TNF-alpha inhibitors.
- The radiographic manifestations of TB and the differences in immunosuppressed hosts.
- The yield of bronchoscopy in patients who are not coughing.
- The potential role for gastric aspirate to make the diagnosis
FYI - Canadian Tuberculosis Standards (Guidelines) available for free here.
Tuesday, January 5, 2010
Streptococcus milleri group
Today we reviewed a case of multiple soft tissue abscesses caused by an organism of the Streptococcus milleri group.
This group of organisms includes:
- S. anginosus
- S. intermedius
- S. constellatus
Because of phenotypic similarities, exact speciation can be difficult without more advanced means of testing. Speciation matters as intermedius and constellatus are very frequently associated with abscess formation; wheras anginosis is not. The clinical presentations of the various species are discussed in this CID article. Soft tissue abscesses are most common, followed by pleuropulmonary (including empyema), intrabdominal (including liver abscess), and brain abscesses.
The propensity to form abscesses may be related to impaired neutrophil chemotaxis and resistance to destruction when phagocytosed.
Treatment involves adequate surgical source control, and antibiotics, usually parenteral beta-lactams such as Penicillin G if the isolate is susceptible. Duration of therapy varies depending on location of abscess and adequacy of surgical drainage.
Monday, January 4, 2010
Staphylococcal bacteremia
Am back on clinical service today! So, I will begin to blog again...
Today we discussed Staphylococcus aureus bacteremia including MRSA. I have previously blogged about this here -- with links to what I believe are the relevant articles.
I will add this article from CID which discusses combination antibiotic therapy in MRSA infections.
Today we discussed Staphylococcus aureus bacteremia including MRSA. I have previously blogged about this here -- with links to what I believe are the relevant articles.
I will add this article from CID which discusses combination antibiotic therapy in MRSA infections.
Subscribe to:
Posts (Atom)